[Research report] COVID-19 Vaccinations and People’s Rights in South Korea
CONTENTS
Chapter 1. Introduction
Chapter 2. Politicization of COVID-19 vaccination
Chapter 3. Political economy of vaccine research and development
Chapter 4. Vaccination Policy and public health care system
Chapter 5. Justice and Ethics of Vaccination
Chapter 6. COVID-19 vaccines: Global governance for global justice
Chapter 7. Civic Engagement in the COVID-19 Vaccine Policy Process
ENGLISH ABSTRACT
Chapter 1. Introduction
Vaccines and publicity are the most frequently mentioned keywords in Korea’s COVID-19 “system.” Vaccines have emerged as a strong alternative or consideration in that they are almost the only way to end the COVID-19 epidemic. The health care system, centered on the private sector, or market principles, has revealed its limitations in the process of responding to COVID-19. The combination of vaccines and publicity, which were other trends of interest, came after major high-income countries predicted to monopolize the COVID-19 vaccine from late 2020. The following perspectives are needed to understand the vaccine problem. First, an important characteristic of vaccines is that it is a ‘product’ that is often traded in the ‘market’ as a result of industrial ‘production’. Second, the so-called “health care system” perspective is also needed in discussions surrounding vaccines and vaccinations in Korea. Third, it is also important to understand vaccines and vaccinations as “the social” beyond science, technology, medicine, and bio-medicine. When the political-economic logic of vaccines and the goals of the COVID-19 response conflict, publicity can serve as a criterion for judging and socially solving them. At this time, publicity includes the nature of practical ethics centered on rights to health, international justice, and distributional justice.
Chapter 2. Politicization of COVID-19 vaccination
Since the COVID-19 outbreak spread, mask-wearing, hand hygiene, and social distancing became the most common measures to prevent the spread of the virus. After the introduction of vaccination, the vaccine has been considered the most effective way to fight the pandemic through herd immunity. Although these preventive measures are based on epidemiological and scientific evidence, some politicians, experts, and the media from countries worldwide, including Korea questioned the potential side effects of vaccines, intentionally stimulating anxiety and fear among citizens. This study regards this phenomenon as a politicization of COVID-19. Politicization is defined as “a dynamic process in which public actors engage in political discourses in the public sphere for political agenda-setting and resource distribution.”
Politicization seems to have negative effects because it may cause social conflicts; however, theoretically, it can have positive effects when various actors expose and magnify problems that have been neglected, then discuss and cooperate to solve the problems in the public sphere. In this process, citizens can participate in health-related decision-making through public discussion. However, if the quality of discussion is not up to standard due to various reasons (e.g., political bias and misinformation), it can result in socially undesirable behaviours such as vaccine hesitancy.
This study derived the following themes of politicization of the COVID-19 through deductive reasoning based on team discussion: vaccines quantity and vaccination schedule, vaccination priority and equity, vaccines safety and the individual right to choose vaccine brands, and the government’s response to adverse reactions from the vaccines.
During this politicization of the COVID-19 vaccine, public actors, including state, economic, and social powers, engaged in political discourses to achieve different goals. The state power emphasized a timely introduction of vaccines and treatments, and support to devise vaccines in cooperation with domestic pharmaceutical companies to gain the legitimacy of governmentality. The state power showed the close relationship between the state and economic powers by setting the goal of the growth of the pharmaceutical industry and market expansion.
Social powers attempted to improve public interests, protect the socio-economically disadvantaged, and protest against international inequality of vaccine accessibility, making them the main political agenda. However, since public health has largely been influenced by state powers, social power has had a relatively small impact on the COVID-19 pandemic. As a result, disagreements arose about various issues such as resource distribution, and subsequently, they led to social conflicts during the politicization of COVID-19.
Chapter 3. Political economy of vaccine research and development
Global healthcare research and development (R&D) framework is working with public funding mechanism including ‘push’ strategy such as research grants or tax breaks, and ‘pull’ strategy such as orphan drugs or advance-purchase commitments. It should be reviewed the power of agents including state, economy and social dimension to understanding the framework. For the political economy analysis of vaccine R&D we examined the state, economic and social power relationship within the R&D framework. In most high-income countries, the state-operated push and pull mechanisms. The economic power transformed their strategy from concentrated investment for R&D to financialization, because the traditional drug markets have gradually deteriorated. The economic power focused on the profit from stock or merge and acquisition, rather than developing new drugs by intensive investment to R&D. Simultaneously, despite the economic power pretend to accept social demands such as corporate social responsibility and to redistribute their wealth via various charity, money to be invested those activities would be re-pocketed into the drug companies. Social power plays a role as a watchdog against R&D activities. The role of the social power in the vaccine R&D framework was only focused on the terminal stage of the R&D process, even if the social power tried to engage in development, design, implementation and accessibility to the end product of R&D. In South Korea, it is also hard to understand why the social power is important or what kinds of role they can do in R&D framework. However, the most important thing is the unfair R&D governance where crucial values including participation and watching were excluded. Frankly speaking, there is no room for social power within the R&D framework in South Korea. Therefore, the agenda of the social power for the future has to re-organize and reconstruct the now unfair R&D framework.
Chapter 4. Vaccination Policy and public health care system
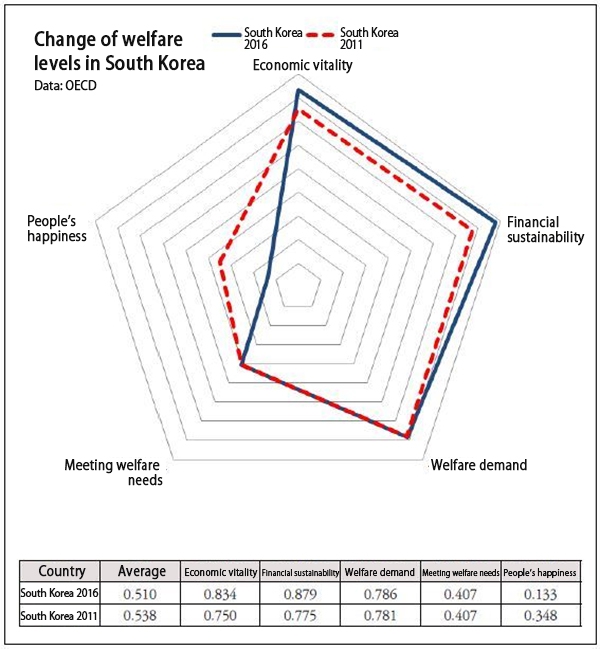
Since the 1970s, many high-income countries have promoted new public management reforms. Based on the belief that the market is more efficient than the government, public services provided by the government were handed over to the private sector, and the government also had to introduce market principles for efficiency. However, there are also strong criticisms that it is difficult to achieve the original purpose of improving the quality of services and reducing costs, and that it can weaken the system. For example, it weakens the expertise, responsiveness, control, and accountability of government agencies, and makes it difficult to solve inequality problems.
In Korea, since liberation in 1945, sufficient expenditure has never been made on the public health care system amid an absolute lack of resources, a developmental state pathway, and a new public management paradigm. Meanwhile, private hospitals overwhelmed public hospitals in quantity and quality, and the public role decreased. Health centers with insufficient manpower and financial input also promoted public-private partnerships as the burden of work increased significantly.
In the vaccination system, the participation of private medical institutions expanded, starting with the pilot project to support essential vaccination costs for private medical institutions in 2005. In the 2019-2020 season, contracted medical institutions accounted for 89.2% of influenza vaccinations for the elderly aged 65 or older.
The contracted medical institutions played a key role also in the COVID-19 vaccination. However, the distribution of locally unequal medical institutions in private-centered systems can also affect vaccination. In addition, it is difficult to properly manage and supervise a significant number of private medical institutions by public health centers that are already overloaded. In the trend of new public management, the decrease in the role of public health centers may gradually lead to a reduction in capacity, authority, and expertise as health authorities.
In order to alleviate current concerns, it is imperative to increase resources such as institutions and manpower in the public sector. However, just because the public sector grows quantitatively does not automatically guarantee public values. If outcome-oriented and efficiency are still the top priority, unequal structures and results are difficult to change. Democratic governance that can reflect the voices of marginalized people and a public-private partnership between state power and social power are needed.
Chapter 5. Justice and Ethics of Vaccination
As vaccines are essential resources to respond to the pandemic, the equitable allocation of vaccines should be considered. However, only healthy maximization from a utilitarian approach is implemented as ethical principles for vaccines allocation in South Korea. This response to the pandemic has exposed existing social inequities and even exacerbated them during the entire vaccination process. Vaccination inequities are reproduced by dynamics of following a triple structure: 1) socioeconomic structure (i.e. social determinants of vaccination accessibilities), 2) policies and institutions (i.e. health care system, and national immunization programs), and 3) culture and an episteme (i.e. exception status, utilitarianism, neoliberalism). Defining the pandemic as an exception status, utilitarian and liberal values that internalize individualization are prioritized over any other values such as equity and justice. In other words, inequities become commonplace thus are treated as unavoidable. Given the situation, individuals should bear any kinds of risks and injustice. Under ‘governmentality,’ only N% of vaccination is set as a top priority goal of the national immunization program. While social determinants of vaccination are not equally distributed, the national immunization program has never considered resolving them as well. Consequently, the structure of vaccination inequalities calls for ‘democratic publicness.’ From this perspective, we believe that vaccination justice could be achieved when the pandemic responses set equity as a top priority principle, establish the procedural ethical framework based on civil societies as a social base, and decentralize the power.
Chapter 6. COVID-19 vaccines: Global governance for global justice
As the COVID-19 is a pandemic, the justice for vaccines must also be considered at the global level across borders. The production and distribution of the COVID-19 vaccines and the pandemic itself are issues of global justice that cannot be settled without joint efforts and that show inequalities between countries.
Through the COVID-19 pandemic, global health governance aims for global health security have revealed various problems. The COVAX was launched to distribute vaccines according to the public health needs of countries, not economic, political, or geopolitical interests, but has degenerated into an aid mechanism due to vaccine nationalism and vaccine diplomacy of the powerful countries. Effective international legal grounds were needed to make the supply of vaccines produced by transnational pharmaceutical companies being under the control of the WHO and the COVAX, but under existing global health governance centered around the International Health Regulations and the WHO, there was no way to do that. Beyond the limits of the current “global health governance,” the “global governance for health” perspective is more relevant than ever in the COVID-19 pandemic. It aims for equitable global governance should be created that considers all political, economic and social determinants affecting health.
Global powers and transnational capital seek to stabilize capital accumulation while responding to their domestic pressure with the COVID-19 vaccines. This motivation makes the achievement of global justice less priority or drags it down as a means for the national interest. Rather than trying to change this global trend, the South Korean government is actively riding on it and seeking to secure economic and technical superiority and stable governmentality with the COVID-19 vaccines and treatments. In order for the government to quickly achieve these goals, it is essential to obtain cooperation from companies, which has led the companies to take the lead in discussions on the development and production of the COVID-19 vaccines and treatments in South Korea.
The last hope lies in the global solidarity movement. In fact, it is only the social movement that can check the national states and governments, which prioritize their domestic politics and governmentality. Since the 1990s, global civil society has continued to fight for global justice insisting on affordable prices for equitable access to medicines, against transnational pharmaceutical companies as well as the intellectual property regime strengthening since the establishment of the WTO. In the COVID-19 situation, South Korean civil society has been striving for equitable access to vaccines around the world by solidarity with the global civil society, criticizing governments and companies.
As of the end of September 2021, the exemption from intellectual property rights through WTO/TRIPs (TRIPs waiver) is the top priority campaign agenda for civil society around the world. The adoption of the TRIPs waiver proposal could be the beginning of just global vaccine governance, in which countries expand the pie themselves instead of competing with each other over the pie set by transnational pharmaceutical companies, and low- and middle-income countries gain rights to vaccine production instead of waiting for vaccine aid from high-income countries.
Chapter 7. Civic Engagement in the COVID-19 Vaccine Policy Process
The purpose of this study is to explore how collaborative governance including civic engagement can be developed in the era of the COVID-19. The findings open up several issues about vaccination policies from civil society perspectives: inequity in vaccine access, the lack of communication between civil society and government, government-led decision-making processes, and the absence of co-production of knowledge. Evaluation of citizen participation related to national advisory committees on vaccination reveals the status of “tokenism”, supported by a window dressing ritual or one-way flow of information. Our findings highlight the constraints on the ‘Political opportunity structures’ and collaborative governance. Even though civil society attempted to construct alternative countervailing power, which lies between adversarial and collaborative one, empowered participatory decision-making did not occur in vaccination policies. Institutional design efforts should be required to advance empowered participatory governance.
Full report (in Korean) download: COVID-19 Vaccinations and People’s Rights in South Korea by PHI & PHM Korea